Mr Martin Smith is a qualified social worker and the Recovery Lead for Substance Misuse Services at Derbyshire Healthcare Foundation Trust (DHCFT). He has twenty-five years of experience working within the substance misuse field and routinely collects patient data, proactively collating available mortality data to attempt to identify patterns in deaths and the ways in which clinical services might mitigate them. He is a member of the NHS Substance Misuse Provider Alliance and was a member of the Advisory Council on the Misuse of Drugs Recovery Committee 2014-2017. He shared this analysis of mortality in the substance misuse treatment population with us.

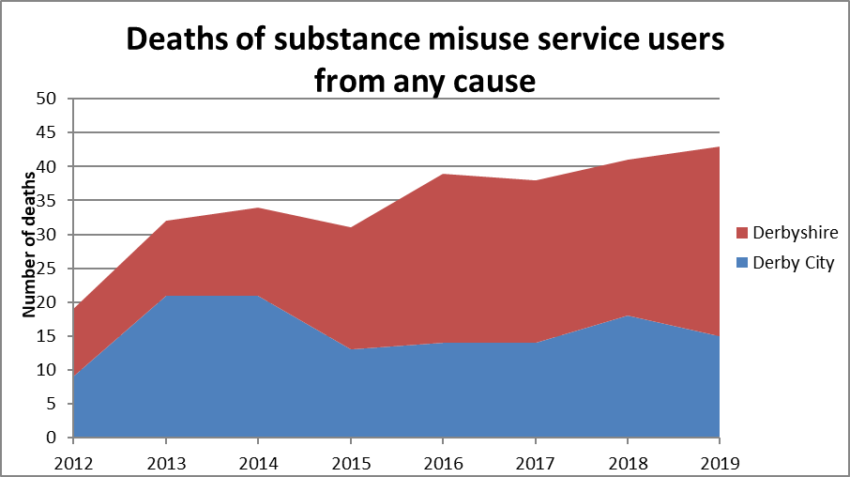
Around 2013-2014, like many in the sector, we began to see a rise in deaths within our services. Like other providers, we were beginning to see a rise in all-cause mortality deaths so we decided to take a closer look. Our task was to investigate the complexity of risk factors for premature all-cause mortality within the treatment population and the impact of current clinical management.
There were 316 deaths of people engaged with Derbyshire Healthcare’s (DHCFT’s) substance misuse services (or up to one-year post-discharge) between 1 January 2012 and 20 August 2020. The data cut of point meant we only had a partial year for 2020 so it wasn’t included but the deaths in 2020 and 2021 exceeded 2019.
Cause of death
Overdose (predominantly opiate) was by far the most common cause (115 cases), constituting 40% of deaths for which the cause was known. The cause of death was unascertainable or not yet known in 21 cases (7%). After heroin or opiate toxicity, drugs such as diazepam, temazepam, gabapentin, mirtazapine and increasingly pregabalin are frequently highlighted under section 1b (‘underlying cause’ of the main cause of death) on the death certificate.
All other deaths are physical health related with the exception of suicides of which there was 20 (6.3%). The most common causes of physical health deaths are predominantly from liver disease, COPD, bacterial infections and cancers.
Age and Gender Profile
The highest number of deaths occurred in the 35-39 years age group, followed closely by the 40-44 years group. This age profile of overdose deaths followed the same pattern, but with a more pronounced peak in the 35-39 years age group. The data suggests that those aged 50 and over are more likely to die from a physical health condition than an overdose. In the 50-plus age group, 19% of deaths were due to overdose, compared to 39% of deaths in those aged 35-49.
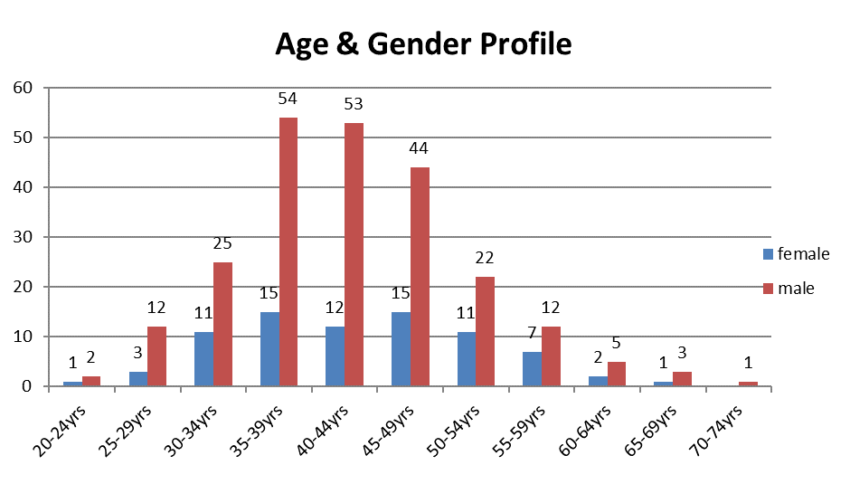
When only chronic causes of death are analysed (brain-related illnesses, cancer, cardiovascular illness, diabetes, liver disease, lung conditions and kidney disease), the age profile becomes slightly older, with a peak in the 45-49 year age bracket. However, the data shows many deaths at a young age from these causes, with 58% of deaths occurring in those aged under 50 and 22% in those under 40.
Circumstances of death
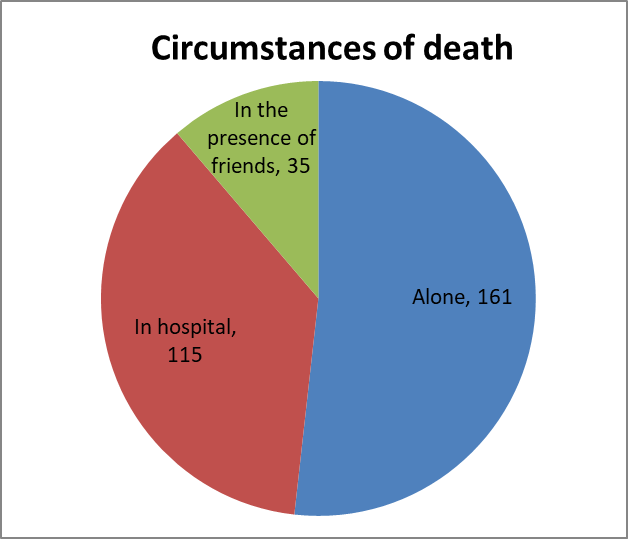
The data shows that most individuals (161; 52%) were found alone, while 37% (115) died in hospital, a hospice or care home. Most deaths in hospital were caused by physical health conditions; only 11 were due to overdose. Twenty-six of the people that died in hospital were receiving end of life care.
Only 11% of all decedents were known to have died in the presence of friends. Of those people who were found alone, 80% were male.
Of those 115 people that died by overdose, an even greater proportion (72%) were found alone. Ten percent of overdose deaths occurred in hospital and 18% in the presence of friends.
Physical health conditions were highly prevalent in the cohort that died, with 81% of people (251) having at least one such condition. 60% of people (186) had two or more conditions.
The most commonly occurring conditions were chronic obstructive pulmonary disease (COPD) at the time of death. In this study, 243 decedents were under the age of 50. Of these 191 had at least one long term health condition such as COPD, liver disease, or a heart condition, and 155 had an identifiable mental health condition, such as anxiety and depression disorders, personality disorder, PTSD and psychotic illness. Poor physical health with many having life-limiting conditions will continue to be a challenge to the sector.
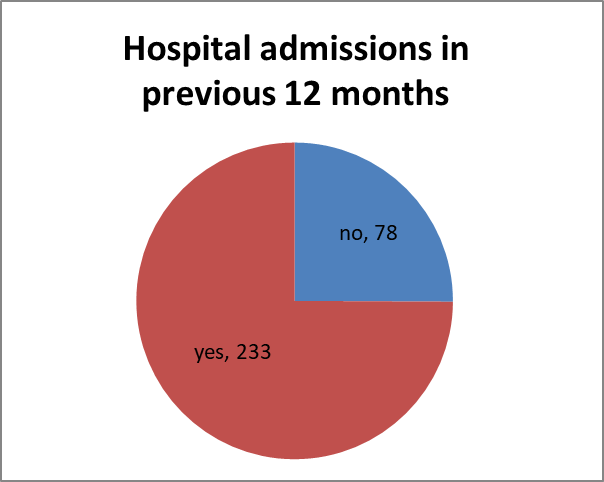
Hospital admissions in the previous 12 months
75% of people who died had had at least one hospital admission in the previous 12 months, A significant red flag and a clear indicator of risk regardless of the reason for hospital admission.
Key findings and red flags
- Male gender (75%)
- Living in isolation (67%)
- Problematic alcohol use (50%)
- Being unemployed or retired (94%)
- Smoking (97%)
- Living in deprivation (77% living in the top 40% most deprived postcodes)
- Current or previous intravenous use (83%)
- Hospital admission/s in the previous 12 months (75%)
- Prison release within the previous 12 months (11%)
- Mental health difficulties (64%)
- Additional prescribed medications (gabapentinoids/benzodiazipines/opiates etc) (71%)
- Comorbid health conditions (81%)
Commentary
In addressing overdoses we started rolling out Naloxone in 2015 and it’s likely that deaths both locally and nationally would have seen a greater increase without it. However, the central premise for naloxone effectiveness is that another person must be present and available to administer it at the time of an overdose. With the number of people using drugs alone, living in isolation, and dying alone it is becoming clear that further interventions will be required. It is highly likely that technology will play a key role with some in the sector taking an interest.
A partnership between Derbyshire Healthcare Foundation Trust and the ImpACT+ (specialist respiratory/COPD) team based at the Royal Derby Hospital was created to address a recognised need for access to specialist respiratory care for those accessing our services. This service is now delivered from within two of our treatment bases. More people have been diagnosed and commenced on treatment regimes. One case of TB has been identified and treated. Many with symptoms but undiagnosed have been identified and received appropriate investigations for symptoms they had previously not addressed or been unable to access their GP to discuss. And one client was identified to be suffering from 4 PEs, a DVT and heart failure and is only alive today because the Health Improvement Nurse had access to the specialist team who were able to act accordingly on her concerns.
We continue to work in collaboration with several ODNs and Hepatitis C peers alongside our nurses to eliminate Hepatitis C which is a risk factor in some deaths. In the last 2 years, only one person had Hepatitis C referenced on their death certificate.
We introduced in Derby on-site ECG testing where tests are uploaded and within 30mins results are received, a recent audit showed 33% needed a follow-up referral, the system is fully integrated with GP/Hospital and our own data system. We will soon be rolling this out across the county.
In order to keep people engaged in treatment, we employed an outreach worker to re-engage those that had dropped off their prescription and stopped attending appointments. Optimisation of medication is encouraged so those in receipt of it can find a dose that is comfortable for them.
Further outreach workers were employed in the city and county to work specifically within the homeless community and in the city, we have an outreach worker to work specifically with females who are at risk.
One of the challenges the sector faces is not just deaths through overdose but deaths through physical health conditions. It sometimes appears that it is acceptable to talk about deaths in general but it’s unusual to see services openly discuss all-cause mortality within their services. As we move into 2022 the full impact of COVID-19 on this client group is currently unknown, but it is reasonable to assume that the isolation and inequalities that they experienced pre-COVID would have intensified throughout 2020-2022. As we all see a rise in the cost of living it is those with the least that will be most affected,
Future research should also examine the impact of opioid substitution treatment on mortality.
Martin Smith Recovery Lead Derbyshire Healthcare Foundation Trust
Register FREE to access 2 more articles
We hope you’ve enjoyed your first article on GE Insights. To access 2 more articles for free, register now to join the Government Events community.
(Use discount code CPWR50)




