This article will examine the latest safety concerns in healthcare, and how best to avoid them.
Sean Weaver, Deputy Medical Director at the Healthcare Safety Investigation Branch (HSIB) discussed Never Events, how to ensure solid improvements following an investigation, and how to embed regular reiteration into the overall strategy.
About the Healthcare Safety Investigation Branch
HSIB carry out independent safety investigations in NHS-funded care in England. They do not apportion blame or liability but focus on system-level change.[1]
Their aim is to professionalise the patient safety investigator role through education, and transparent and collaborative support. They have wide-ranging expertise from safety-critical industries such as aviation and rail.
The multidisciplinary team emphasise the importance of patient and family involvement in the process, ensuring that learning is the main focus rather than attributing blame.
HSIB’s investigation programmes are split into two main themes; national investigations and maternity investigations.
National Investigations Programme
- Core purpose outlined in 2016
- Diverse range of healthcare services and safety risks covered
- Tasked with deciding the scale and risk of harm
- Uncover potential for learning to prevent future harm
- Assess the impact on individuals and public confidence in the healthcare system
- Running up to 30 investigations a year (not replacing local investigations)
- 85 investigations carried out to date with 89% family engagement
- Making recommendations to healthcare services (and beyond where necessary)
- Publishing reports on HSIB website
Maternity Investigations Programme
- Specific programme added in 2018
- Explicit focus on maternity services in England
- Looking at the Each Baby Counts programme
- Calculate direct maternal deaths
- Assess indirect maternal deaths while pregnant or within 42 days of giving birth
- Carrying out roughly 1000 investigations a year, replacing local investigations
- 2881 investigations carried out to date with 87% family engagement
- Recommendations made only to the trust
- Reports belong only to the family and the trust
Through these two branches of their work, the aim of HSIB has been to improve patient safety.
Throughout their findings, they have found the best way to achieve this is through plenty of patient and staff engagement, analysing a lot of human factors with a lot of different backgrounds, and integrating this into a systems approach.
Never Events
In the Institute of Medicine’s report ‘To Err is Human’, published in 2000, it was reported that between 50,000 to 100,000 deaths in US healthcare were due to adverse events every year.[2]
The report claimed that over half of these resulted from medical errors and could have been prevented.
In 2002 the National Quality Forum coined the term Never Event in reference to “particularly shocking medical errors such as wrong-site surgery.”[3]
Lord Darzi’s High-Quality Care for All report in 2008 recommended that a Never Event list be developed for the NHS.[4] The original criteria were set out which an incident had to fulfil to be classified as a never event. This included:
- Having clear potential for, or has caused severe harm or death
- There is evidence of the risk occuring in the past
- There is existing national guidance or national safety recommendations on how the event can be prevented
- The event is largely preventable if the guidance is implemented
- Occurence can be easily defined, identified, and continually measured
The NHS Never Events list was launched in 2009, following the definition “serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers”[1]
The original ‘core eight’ list of never events were:
- Wrong site surgery
- Retained instrument post-operation
- Wrong route administration of chemotherapy
- Misplaced naso or orogastric tube not detected prior to use
- Inpatient suicide using non-collapsible rails
- Escape from within the secure perimeter of medium or high secure mental health services
- Patients who are transferred prisoners (not included in the previous contractual list)
- In-hospital maternal death from post-partum haemorrhage after elective caesarean section
- Intravenous administration of mis-selected concentrated potassium chloride [5]
Both the list of never events and the definition has evolved over time, and was revised by NHS Improvement in 2018.[6]
They tweaked the definition to:
“patient safety incidents that are wholly preventable where guidance or safety recommendations that provide strong systemic protective barriers are available at a national level and have been implemented by healthcare providers.”[6]
NHS Improvement 2018

HSIB has carried out 10 national investigations focusing on 7 Never Events.

HSIB has carried out three investigations into wrong-site surgery, two into wrong implant/prosthesis, and one each for the remaining five never events.
HSIB’s Approach to Increasing their Impact
HSIB set out to make stronger recommendations and increase their impact on the reduction and prevention of Never Events.
They incorporated the theory of Systems Engineering Initiative for Patient Safety (SEIPS) into their strategy, which is a systematic qualitative analysis of the themes in the workplace that contribute to Never Events occurring.[1]

Whilst the above breakdown is simplified, the findings when implementing this into investigations are incredibly complex.

HSIB found 17 themes contributing to Never Events. The barriers for these events were neither strong nor systemic, and therefore these events do not fit the definition of Never Events as they are not ‘wholly preventable.’
One example found during an investigation was the wrong application of screws. Whilst there was no damage to the patient, this technically classed as a Never Event.
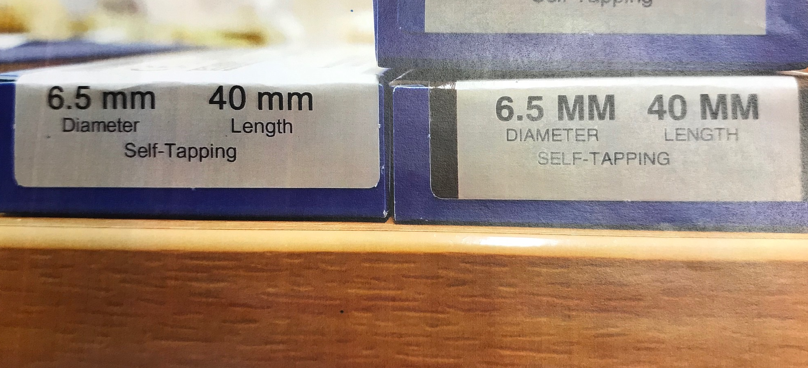
The inclusion of this image in their investigation sought to highlight that healthcare staff dealing with personal protection equipment at the height of the pandemic, operating under sub-optimal conditions, cannot be blamed for this kind of mistake.
To account for this, there are five kinds of barriers that can be put in place.

Elimination
This involves redesigning to remove the hazard completely.

Substitution
Replacement of the hazard with something less dangerous.

Engineering
Use of new redesigned equipment to prevent an accident.

Administrative
Identifying and implementing procedures to work safely.

Protective
If the above options aren’t possible, protective barriers rely on behaviour change to protect patients and staff.
An example of a protective barrier could be the introduction of checklists. Whilst they do promote the safer practice, they cannot be quantified as providing a strong and systemic barrier and do not make something wholly preventable.[1]
Recommendations and Conclusions
HSIB has put forward three recommendations concerning Never Events following their investigations.
Recommendation 1 “It is recommended that NHS England and NHS Improvement revises the Never Events list to remove events, such as those presented in this national learning report, that do not have strong and systemic safety barriers.”
Recommendation 2
“It is recommended that NHS England and NHS Improvement develops and commissions programmes of work to find strong and systemic barriers for specific incidents where barriers are felt to be possible but are not currently available.”
Recommendation 3 “It is recommended that the Centre for Perioperative Care reviews and revises the National Safety Standards for Invasive Procedures policy to increase standardisation of safety-critical steps that are common across all procedures.”
To conclude, HSIB observed that:
“It would be beneficial if significant safety events, such as those presented in this national learning report, continue to be reported and investigated by NHS organisations without apportioning blame or liability, using a recogniszed systems-based approach such as SEIPS as used in this report.”
HSIB
[1] Weaver, Sean. 2021. Deputy Medical Director, Healthcare Safety Investigation Branch. Creating Regulation to Support Healthcare Workers Achieve Better Outcomes.
[2] National Library of Medicine. 2000. To Err is Human: Building a Safer Health System.
[3] National Quality Forum. 2002. Never Events.
[4] Lord Darzi. 2008. High Quality Care for All: NHS Review.
[5] NHS.co.uk. 2008. Core Never Events.
[6] NHS.co.uk. 2018. NHS Improvement Policy Proposals.
Register FREE to access 2 more articles
We hope you’ve enjoyed your first article on GE Insights. To access 2 more articles for free, register now to join the Government Events community.
(Use discount code CPWR50)




