The National Institute for Health and Care Excellence published its Quality Standard on Sexual Health in 2019 [1]. It reiterates the importance of promoting first-rate sexual health as well as reinforcing the need to maximise access to Long-Acting Reversible Contraception (LARC).
Poor sexual health can lead to unintended pregnancies as well as sexually transmitted infections. Research conducted by Bentley et al [2] draws a link between social class and contraception uptake, demonstrating that women in lower socioeconomic areas are less likely to use contraception than women in advantaged areas.
The Strategy of Liverpool City Council
James Woolgar is the Advanced Public Health Practitioner and Sexual Health Lead for the Public Health Department at Liverpool City Council [3]. They spoke to us about the work that Liverpool is doing to improve access to LARC and the development of Women’s Reproductive Health Hubs.
Liverpool is England’s 6th largest city with a population of 498,048. The population has risen by 12.6% since 2009. There are areas of deprivation with high teenage pregnancy rates, as well as high abortion rates. The city has seen a significant rise in women of child-bearing age, bucking the national trend for the number of males and females who need to have access to contraception.
Consequently, Liverpool City Council’s overarching vision involves:
- Improving access and uptake of LARC methods for women in Liverpool
- Improving GP provisions for intrauterine systems, facilitating the management of common gynecological conditions closer to home
- The development of a Women’s Health Hubs approach in General Practice
- Ensuring that services are working intelligently and together to provide seamless access to the correct type of service for each and every condition
The three-year vision for sexual health services in Liverpool:
- To expand the reproductive health offer in General Practice
- To ensure the use of reproductive coils for full extended benefit so that their distribution is not restricted
- To increase the amount of LARC prescriptions distributed
- To improve accessibility, proximity of services and choice for women
- The creation of greater appointment availability by increasing system capacity
- To reduce wait times (currently between 2 – 4 weeks)
Reproductive Health Hub Approach
The reproductive health hub approach brings together four core services – Contraception, Emergency contraception, Menopause Management and Heavy Menstrual Bleeding (HMB) treatment. James promotes the hub model as being flexible enough to suit any local system.
The key aim of combining these core services is to bring convenient access to women in Liverpool. The service is fully connected with Liverpool Women’s Hospital. Services currently include:
- Cervical Smears (Cytology)
- Community Gynecology (included HMB treatment)
- Menopause management
- Fitting ring pessaries
- LARC distribution
- Sexual health advice
There are future plans to include a specialised Menopause service as well as a Polyps removal service.
Why is this Vital?
Liverpool City Council decided that it was vital to provide an accessible health hub upon reading the latest guidance and policy direction surrounding sexual health in the UK.
The Better for Women report published in 2019 by the Royal College of Obstetricians & Gynecologists (RCOG) [4] called for the creation of national strategies for women’s health based that are based on a life course approach to address areas of unmet need.
The RCOG also inspired Liverpool to find ways to provide easier access to contraception, abortion and fertility services. They called for service providers to note missed opportunities and barriers to women accessing contraception, in particular LARCS. Better contraceptive advice and counselling is also needed according to RCOG.
An audit conducted by the Faculty of Sexual and Reproductive Healthcare (FSRH) in 2019 of emerging new models of care has found that only a quarter of the new models mentions contraceptive services and/or community gynaecology in their plans.
This was noted by Liverpool City Council and James explains that this compelled them to create the Women’s Health Hub for the women of Liverpool.
The audit reviewed more than 50 strategies and operational plans, with results showing that few areas have explicitly recognised the opportunity to embed sexual and reproductive healthcare services in their strategies.
Primary Care Network Formation – The Liverpool Model
The new model of care in Liverpool will allow for a more integrated relationship between the Liverpool Women’s Hospital, GP’s and Community Sexual and Reproductive Health Services. The Women’s Health Hubs operate within a new primary care network foundation in Liverpool.
Lower risk and common gynaecological conditions will be managed in primary care and community services. Complex and higher risk conditions will be referred to Liverpool Women’s Hospital and the hospital will facilitate training and support to GP’s via city-wide education and training groups.
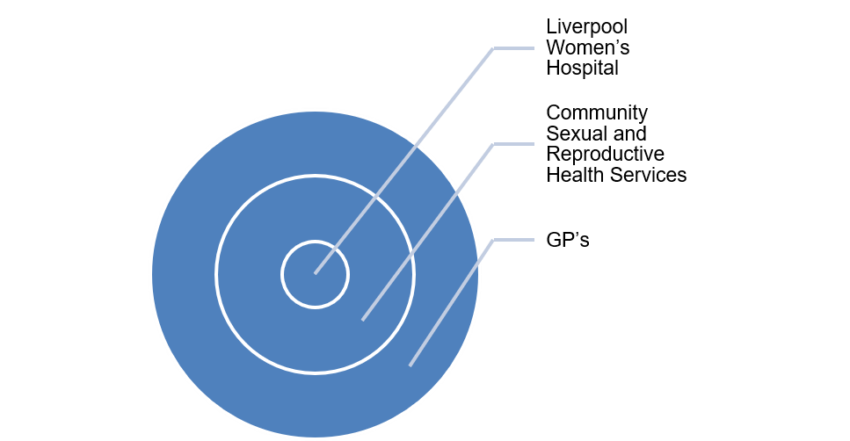
There are currently 10 Women’s Health Hub networks across Liverpool. Women will be able to book into services via their GP or by self-referral.
Selected Hubs have been commissioned to undertake the bulk of LARC distribution. To do this, audits were completed at practices to see if they were the right fit for this responsibility. The assessments involved identifying the current level of activity within the practice.
The Hubs all share the same IT system – EMIS Inter-Operability. All practices share the same centralised appointment booking record and any practice can book into any cross-service slot.
Additionally, there has been an investment in the training of new LARC fitters. There is a minimum of 30 places available annually for GPs to train to gain LARC fitting competencies. This training is free.
The new system is being communicated across Liverpool via posters, leaflets, texts to patients and targeting those women who access the services but are not currently using LARC.
James states that the collaboration of services makes the Women’s Health Hub a system that is easy to control. It aims to make patients feel safe in the service they have been referred to; through seamless referrals and clear communication between services. Additionally, it will mean that patients aren’t waiting weeks to be seen by a service.
Impact to Date
Croxteth and Norris Green are areas of Liverpool that were among the first to adopt the new systems. There are 6 practices covering this area, catering to 36,000 people. Early results show that the model is proving successful in the uptake of LARC:
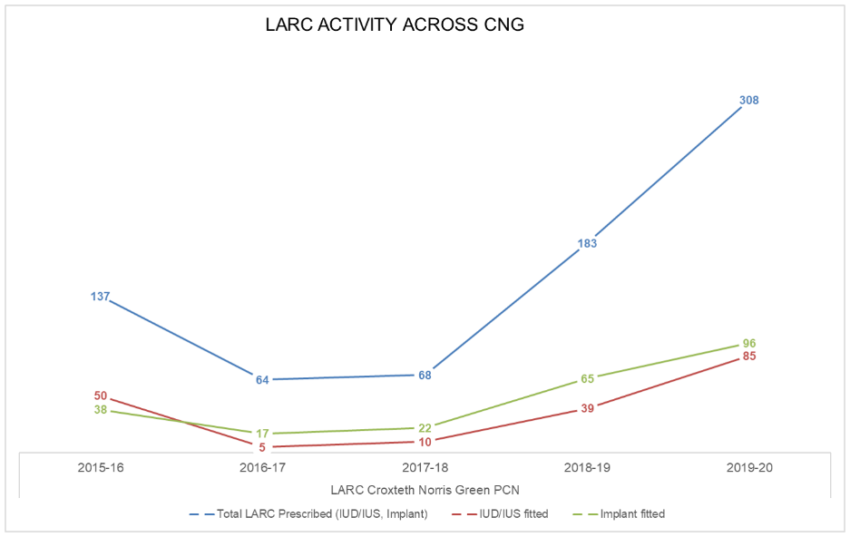
In the Croxteth and Norris Green areas, there has been a clear increase in the fitting of LARC prescribed implants.
James explained that the new system has significantly shortened waiting times. Additionally, they estimate that increase in LARC distribution has saved 415 unintended pregnancies. This equates to £1m savings to NHS in cost modelling and £4.5m total social care costs.
Additionally, women suffering from Heavy Menstrual Bleeding are now being referred to the correct service at Liverpool Women’s Hospital instead of a GP. This has saved over £120k per annum in referral costs.
On a regional Merseyside basis, £300k has been saved in unnecessary appointment/referral costs. This makes a clear case for a partnership investment and co-commissioning and collaboration opportunities.
[1] The National Institute for Health and Care Excellence. 2019. Quality Standard on Sexual Health
[2] Bentley R, Kavanagh A, Smith A. 2019. Area disadvantage, socioeconomic position and women’s contraception use: a multilevel study in the UK. BMJ Sexual & Reproductive Health
[3] Woolgar, James. 2021. Advanced Public Health Practitioner for Public Health Department and Sexual Health Lead at Liverpool City Council
[4] Royal College of Obstetricians & Gynaecologists. 2019. The Better for Women report [5] Faculty of Sexual and Reproductive Healthcare (FSRH). 2019. FSRH press release: New models of care could be missing
Register FREE to access 2 more articles
We hope you’ve enjoyed your first article on GE Insights. To access 2 more articles for free, register now to join the Government Events community.
(Use discount code CPWR50)



